The Autonomic Nervous System
The autonomic nervous system is involved in the control of the heart, glands and smooth muscles of the body and plays a major role in regulating unconscious, vegetative functions. It works together with the endocrine system to control the secretion of hormones and is itself controlled by the hypothalamus. Although the autonomic nervous system is considered to be one of the three main divisions of the human nervous system in its own right, parts of both the central nervous systems and the peripheral nervous systems play a role in its functions. The autonomic nervous system has two components, the sympathetic system and the parasympathetic system. These two aspects have antagonistic functions. The autonomic nervous system consists of four chains of nuclei or ganglia, two of which are located on either side of the spinal cord. The outer chains of nuclei form the parasympathetic division of the system while those closest to the spinal cord make up its sympathetic element.
Autonomic Dysreflexia & Hyperreflexia
Autonomic Dysreflexia, also known as Hyperreflexia, is a potentially life threatening condition which can be considered a medical emergency requiring immediate attention. It occurs where the blood pressure in a person with a spinal cord injury (SCI) above T5-6 becomes excessively high due to the over activity of the Autonomic Nervous System.
The most common symptoms of autonomic dysreflexia are sweating, pounding headache, tingling sensation on the face and neck, blotchy skin around the neck and goose bumps.
Not all the symptoms always appear at once, and their
severity may vary. In untreated and extreme cases of autonomic dysreflexia,
it can lead to a stroke and death. Autonomic Dysreflexia is usually caused
when a painful stimulus occurs below the level of spinal cord injury.
The stimulus is then mediated through the Central Nervous System (CNS)
and the Peripheral Nervous System (PNS). 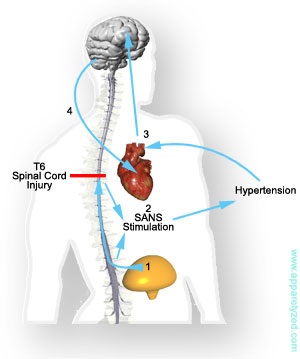
The CNS is made up of the spinal cord and brain, which control voluntary acts and end organs via their respective nerves. The PNS is made up from 12 pairs of cranial nerves, spinal nerves and peripheral nerves. The PNS also is divided into the somatic nervous system and the autonomic nervous system. The autonomic nervous system is responsible for the signs and symptoms of autonomic dysreflexia. The autonomic nervous system normally maintains body homeostasis via its two branches, the parasympathetic autonomic nervous system (PANS) and the sympathetic autonomic nervous system (SANS). These branches have complementary roles through a negative-feedback system; that is, when one branch is stimulated, the other branch is suppressed.
The SANS is associated with the flight-or-fight response, causing dilation of the pupils, increased heart rate, vasoconstriction, decreased peristalsis and tone of the gut, release of epinephrine and norepinephrine, as well as other effects. The effects of PANS stimulation are the opposite of the SANS; for the most part, these are constriction of the pupil, decreased heart rate, as well as increased peristalsis and tone of the gut.
The PANS and SANS exit at different sites in the CNS. The PANS exits via the midbrain, pons, medulla (cranial nerves [CN] III, VII, IX, and X), and the sacral level of the spinal cord. The SANS exits via the thoracic and lumbar segments of the spinal cord. There is a major sympathetic output (called the splanchnic outflow) between T5 and L2.
In someone with a high-level SCI, intact lower motor neurons sense the painful stimuli below the level of injury and transmit the message up the spinal cord (see diagram). At the level of the SCI, the pain signal is interrupted and prevented from being transmitted to the cerebral cortex. The site of the SCI also interrupts the two branches of the autonomic nervous system and disconnects the feedback loop, causing the two branches to function independently.
The ascending information reaches the major splanchnic sympathetic outflow (T5-T6) and stimulates a sympathetic response. The sympathetic response causes vasoconstriction, resulting in hypertension, pounding headache, visual changes, anxiety, pallor, and goose bumps below the level of injury. This hypertension stimulates the baroreceptors in the carotid sinuses and aortic arch. The PANS is unable to counteract these effects through the injured spinal cord, however. Instead, the PANS attempts to maintain homeostasis by slowing down the heart rate. The brainstem stimulates the heart, through the vagus nerve, causing bradycardia and vasodilation above the level of injury. The PANS impulses are unable to descend past the lesion, and therefore no changes occur below the level of injury.
There can be many stimuli that cause autonomic dysreflexia. Anything that would have been painful, uncomfortable, or physically irritating before the injury may cause autonomic dysreflexia after the injury.